Introduction
Tuberculosis constitutes an extraordinary significant social problem for the population in all over the world. Countries of the Western Pacific reported 1.3 million registered cases of morbidity as of 2013 [1]. As to the South Asia, Pakistan with population of 179.2 million people ranks 5th among 22 countries of the region, with the prevalence rate 231 per 100,000 population [2]. In 2016, 10.4 million estimated new cases of Tuberculosis and 600,000 new cases with rifampicin resistance (the most potent first-line drug) were revealed worldwide. Overwhelming majority of cases (90%) in 2016 occurred in adults, and almost two-thirds took place in seven countries: India, Indonesia, China, Philippines, Pakistan, South Africa and Nigeria [3]. The situation in Europe looks somewhat better, but tuberculosis is quite common here as well. The epidemiological surveillance in Spain showed that the incidence of tuberculosis in 2015 was 10.59 per 100,000 inhabitants [4].
However, one of the tasks within the SDGs (Sustainable Development Goals) of the United Nations for 2015-2030 is the elimination of global epidemic of tuberculosis. The WHO (World Health Organization) strategy on tuberculosis elimination 2016-2035, which is approved by WHA (World Health Assembly) in 2014, urges that the number of deaths from tuberculosis to be reduced by 90% by 2030, and the tuberculosis morbidity by 80% in comparison with 2015 [5]. In the meantime, epidemiological status of tuberculosis across all post-soviet countries still is remained tense. For instance, in the Russian Federation, according to N.N. Drobot et al., a large proportion of children under the age of 2 years have been revealed among the diseased – 17.8%, with 55.8% morbidity rates amongst adolescents, besides, bacterial excretion has been recorded in 30% of cases [6]. Obviously, the Republic of Kazakhstan is not exclusion in the range of post-soviet countries and its epidemiological situation is similar with the borderline Russia.
As well known, the tracing main features of epidemiological process is impossible without the reviewing and prediction the main disease indexes. For the correct epidemiological prognosing of the morbidity on the regional scales, it is necessary to properly fill in the Register, which is difficult when the data are insufficiently collected. The urgency of proper data collection for all nozologias, in particular, for Cancer was discussed in Astana, on 22-26.09.2014, in frames of the first IARC (International Association of Cancer Research) courses for Russian-speaking participants, where Recommendations [7] were elaborated to improve the completeness and quality of Cancer registration in post-soviet countries. These recommendations include facilitating access to the registry and standardizing the information in accordance with current WHO guidelines for international comparability (incidence, mortality, monitoring, patient data, use of special computer programs). The same is of utmost importance concerning tuberculosis as well.
For example, in order to calculate the DALY and QALY indicators that characterize the level of the healthcare system as a whole and the quality of care, it is necessary to record patients’ individual data, along with permanent monitoring (turnover, number and duration of hospitalizations, type of treatment etc.). Regrettably, recommended by the WHO the Astana Recommendations have not yet been implemented in the country. In the meanwhile, state of the Tuberculosis morbidity across the Aktobe province (western Kazakhstan) has been remained tense for past decades and calls for epidemiological analysing and prognosing.
Thus, due to the lack of properly collected full data on the tuberculosis patients, the present research is aimed and implied general evaluation of the tuberculosis key indexes across the Aktobe province during the decade 2008-2017 comparing with the same ones in the country.
Material and Methods
In frames of the present research we found quite appropriate to provide basic data for the country as a whole and for the Aktobe province in particular.
General information: the population of the Republic of Kazakhstan as of 01.01.2016 is 17,417,673 people. Population of the Aktobe region: total – 822,522; urban – 510,568.
The common ratio of men and women is 48%/52%.
The Republic of Kazakhstan ranks 64th in terms of population in the world and 184th in density (6.3 people/sq km). The share of the population aged 15 to 65 is 71%. The national composition: Kazakhs – 66.1%; Russians – 21.5%; other ethnic groups – 12.4%.
The data are taken from: "The population of the Republic of Kazakhstan by regions, cities and districts as of 01.01.2016" of the Committee on Statistics of the Ministry of National Economy of the Republic of Kazakhstan.
Statistical information on tuberculosis cases which has been requested in the Public Health Department of the Aktobe province and in the Public Health Committee of the Health Ministry, used as inputs. Dynamics of the tuberculosis incidence during the last 10 years across the country and the province, including the urban and countryside population, has been studied, with the trends of morbidity determined by the least squares method, according to the formula:
y = a + bx (1),
where y is the leveled indicator; x is the conditional series of numbers symmetrically located with respect to zero; a – conditional mean; b – equalization factor.
Average annual rates of growth (Тgr) were determined.
Thus, the study has been performed retrospectively based on some available official data recorded in the Tuberculosis register. Results obtained have been processed by statistical software package Statistica 10 (USA, Statsoft – Dell Inc.).
Results
Despite the fact that epidemiological situation on tuberculosis still remains tense, a tendency to stabilization and even a reduction of some indicators by 2017 has been noticed.
The number of the tuberculosis cases in the country over the past 10 years has fallen by 58.4%, reaching 52.2 per every 100,000 population in 2017 (compared to 125.5 in 2008, Figure 1).

Figure 1. The incidence rates of tuberculosis in the Republic of Kazakhstan for 2008-2017 per 100,000 population. The data have been taken from the Tuberculosis Register of the Republic of Kazakhstan.
However, rate of the morbidity decrease in the Aktobe province is considered more slow than in the Republic of Kazakhstan in whole: 57.8 vs. 103.0, or decrease by 44.4% (Figure 2).
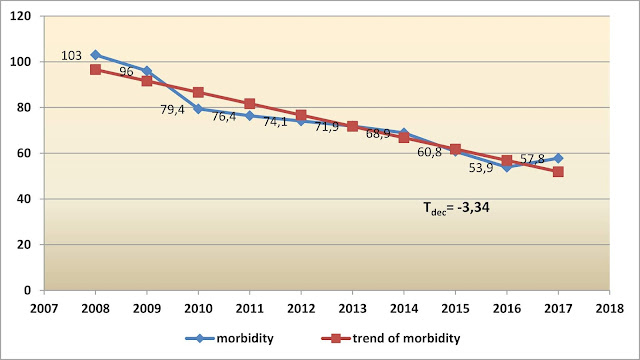
Figure 2. The incidence rates of tuberculosis in the Aktobe province for 2008-2017 per 100,000 population. The data have been taken from the Public Health Department of the Aktobe province (Kazakhstan).
Correspondingly, the trend of morbidity growth across the Aktobe province is relatively slow too, compared to the republican index (-3.34 vs. -4.87).
Obviously, morbidity of 52.2 cases per 100,000 population in our country reached by 2017, still is far from the average incidence rates of the presented countries and the gap will hardly be overcome in the nearest decade.
Comparative data on the different strata of population indicate that the morbidity amongst the urban inhabitants is much higher than in the countryside population across the Aktobe province: 61.6 vs. 51.4 in 2017 (Figure 3). Besides, a large discordance in the rate of the morbidity’s decrease is traced: from 152.3 to 61.6 in urban population (impressed decrease by 59.6%), whereas despite the overall fall by 43.9% in countryside, some growth has been outlined during the last year.

Figure 3. The incidence rates of tuberculosis in the Aktobe province across the urban and countryside population for 2008-2017 per 100,000. The data have been taken from the Public Health Department of the Aktobe province (Kazakhstan).
As aforementioned repeatedly, imperfect filling in along with impeded access to the Register do not allow assess the mortality reasons due to tuberculosis across both the Aktobe province and the country in whole. Nevertheless, information on key indexes is available. So, as to the mortality caused by tubercular infection, positive downward trend has been traced. The death rate distinctly, in 6.3 times, decreased in the Aktobe region over the past ten years – from 17.1 in 2008 to 2.7 in 2017 per 100,000, at that outstripping the national index 3.6 (Figure 4).

Figure 4. Dynamics of the mortality due to Tuberculosis in the Republic of Kazakhstan and in the Aktobe province for 2008-2017 per 100,000 population. The data have been taken from the Public Health Department of the Aktobe province and Tuberculosis Register of the Republic of Kazakhstan.
To our knowledge, the modern pandemic of tuberculosis is featured by increasing the number of destructive forms, due to the growth of mycobacterium genetic mutations with the multidrug resistance. Besides, adverse clinical structure has an impact on effectiveness of the tuberculosis treatment. In Australia, for example, about 1-2% of notifications per a year are classified as multidrug-resistant cases, but such a figure is considered low compared to international standards [8]. As to the state of affairs in our country, specific gravity of destructive forms being 31.4% in 2011 remained almost the same in 2016 (31.3%) in the Aktobe province. And yet, according to data provided by the Public Health Department of the Aktobe province, the closure of the decay cavities, being 73.8% in 2011 has increased up to 85.0% in 2016 ( raise by 11.2%), and bacterial excretion has fallen from 81.4% in 2011 to 61.0% in 2016 (20.4% decrease), respectively. Regrettably, there is no information concerning the drug-resistant forms of tuberculosis across the Aktobe province, and, respectively, there is no opportunity to analyse such an important index. Reportedly, only one of five persons of the estimated number of people with drug resistant tuberculosis has received treatment worldwide [3].
Preventive screening of the new tuberculosis cases constitute a separate large topic within a set of issues concerning the disease dissemination. In the Aktobe region specific gravity of the first time diagnosed cases revealed through the preventive screening, being 66.8 per 100,000 in 2011, decreased to 61.2 in 2016, while the republican indexes were 52.8 and 50.9, respectively.
As known, home contacts are one of the most significant ways of the disease spread out. Information on the disease dissemination ways in the Aktobe region is also unavailable, along with the proportion of the local inhabitants and non-residents (migrants, persons from the correctional institutions and etc.) with the first time diagnosed tuberculosis cases.
Discussion
Basically, global trends in tuberculosis in various countries and regions are featured by a decline. However, 6.3 million new cases were registered globally in 2016 by developing countries that accounted for 61% of the estimated morbidity rate [3]. In Poland by 2015 the incidence rate was calculated as 16.7 cases per 100,000 (6,430 cases), and the rates ranged from 8.3 to 26.5 per 100,000 population in different counties. With that, the average annual decline in the incidence of tuberculosis in 2011-2015 reached 5.5% [9]. In 2017, 9,093 new cases of the disease have been registered in the United States, or 2.8 per 100,000, and being compared to 2016, the incidence decreased by 2.5%. Nonetheless, to achieve tuberculosis elimination by 2100, a steady annual decline in 3.9% is needed [10]. Australia has achieved good results concerning tubercular infection since the mid-1980s, maintaining a low annual tuberculosis incidence rate of approximately 5-6 cases per every 100,000. In 2014, the National Disease Surveillance System received 1,339 reports of tuberculosis, or 5.7 per 100,000 population [8].
Generally, a tendency towards discordance in urban and countryside's morbidity concerning tubercular infection is common. So, the tuberculosis incidence in Poland as of 2015 in the rural population was lower than in cities, respectively 16.5 and 16.9 per 100 000 population [8]. Such discordance in morbidity might be referred to the relatively high density of population in cities, what was reflected in majority of publications on the topic. Besides, there has been noticed that introduction of antimicrobial therapy under conditions of urbanic overcrowding, commonly inherent to developing countries, can even provoke an increase in drug-resistant tuberculosis [11].
Overall, in 2016 1.7 million deaths from tuberculosis had been registered worldwide. With that, the death rate per 100,000 people has been reduced by 3.4% per a year, and the incidence rate by 1.9% per a year respectively, owing to achieved progress in a system of prevention measures. Since 2000 to 2016, the annual global number of deaths from tuberculosis decreased by 24%, and the death rate decreased by 37% respectively. As estimated, 53 million deaths have been prevented by successful treatment worldwide [3]. Such a positive dynamics took place mostly in European countries. Reportedly, in Poland by 2014 specific gravity of the mortality rate due to tuberculosis was at most 0.14% of total mortality. Of total 526 deaths due to tuberculosis in 2014, or 1.4 per 100,000, overwhelming majority died from pulmonary and 22 (4.2%) from extrapulmonary tuberculosis [9].
Issues regarding clinical structure of mortality reasons due to TB are contraversially reflected in the literature sources. A retrospective study of 1,304 adults with tuberculosis who died before completion of treatment in 2005-2006 in thirteen US States revealed that only 72% of deaths were associated with tuberculosis and the rest 28% allegedly related to the disease occurred due to other reasons. Besides, other interesting results were obtained in this study. New risks of death due to tuberculosis during the treatment have been identified: the absence of pyrazinamide in the initial mode (aOR=3.4, 95% CI =1.9-6.0); administration of immunosuppressants (aOR=2.5, 95% CI =1.1-5.6); incomplete diagnosis of tuberculosis (aOR=2.2, 95% CI =1.5-3.3) and alternative non-tuberculosis diagnosis before exact tuberculosis diagnosis (aOR=1.6, 95% CI =1.2-2.2) [12].
Awareness on details of the disease spread out might be much contributed to the in-time correction of region-scale preventive strategies. For instance, in Australia overwhelming majority of tuberculosis cases (84.2%) turned to be persons born abroad. The most common risk factor for tuberculosis infection in people born in Australia was close / home contact with a patient (30.8%) [13]. In Brazil, in 2013-2014, 1,764 cases of tuberculosis were revealed, of them approximately 79% were Brazilians, and the rest were not local inhabitants, and about 30% of all persons had five or more home contacts [14].
According to the long-term goals of the strategy for eradication of tuberculosis (i.e., for 2030 and 2035) developed by the WHO, the public health strategy should be revised to drastically change the current situation on tuberculosis in the world. Comprehensive care and patient-centered prevention should be supported by comprehensive clinical guidelines and standards for the management of patients. Attention should be focused in diagnosis (i.e., molecular methods) and treatment of patients who are difficult to treat, especially those with drug-resistant tuberculosis [15].
Conclusion
Thus, stabilization and relatively steady trend to improvement of epidemiological situation in respect of tuberculosis among the Aktobe population can be stated. There is a noticeable decreasing of both morbidity and mortality rates (morbidity decrease by 44.4% by 2017; mortality rate decreased in 6.3 times). There is a positive dynamics relating destructive forms: the closure of the decay cavities raised by 11.2%, bacterial excretion decreased by 20.4%.
Despite all imperfections in solution of a set of issues relating the tubercular infection, there should be admitted that systematic measures taken by the Health Ministry and local executive authorities contributed significantly to the improving of epidemiological situation in respect of tuberculosis across the country.
Proper filling in the Register and bringing it to international standards are urgently needed, provided we really intend to reduce drug resistance by introducing a patient-centered approach.
Limitations
As mentioned above, the present study constitutes a kind of an initial approach to the due analysis of epidemiological situation in the region. Accordingly, the study is far from comprehensive and has a lot of limitations. For instance, key data on age- or gender-specific analysis of morbidity and mortality have not been presented due to unsatisfactory filling in and impeded access to the Register. The same is concerned to the issues of drug-resistant clinical cases on which information is unavailable.
Acknowledgements
This research was performing in the Epidemiology Department by faculty members of the West Kazakhstan Marat Ospanov State Medical University (Aktobe, Kazakhstan). No funds or sponsoring bodies were involved.
Authors express their gratitude to the staff of the Public Health Department of the Aktobe province (Kazakhstan) for providing a set of data from the Tuberculosis Register to perform a research on the burning topic of the republican Healthcare.
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any stadies with human participants or animals performed by any of the authors.
- Hiatt T, Nishikiori N. Epidemiology and control of tuberculosis in the Western Pacific Region: update with 2013 case notification data. Western Pac Surveill Response J 2016; 7(2): 41-50. https://dx.doi.org/10.5365/WPSAR.2015.6.4.010.
- Khan AH. Tuberculosis control in Sindh, Pakistan: critical analysis of its implementation. J Infect Public Health 2017; 10: 1-7. https://dx.doi.org/10.1016/j.jiph.2016.02.007.
- Floyd K, Glaziou P, Zumla A. The global tuberculosis epidemic and progress in care, prevention, and research: an overview in year 3 of the End TB era. FRCP. Lancet Respir Med 2018; 6: 299-314. https://doi.org/10.1016/S2213-2600(18)30057-2.
- Cano-Portero R, Amillategui-Dos Santos R, Boix-Martínez R, Larrauri-Cámara A. Epidemiology of tuberculosis in Spain. Results obtained by the National Epidemiological Surveillance Network in 2015. Enferm Infecc Microbiol Clin 2018; 36(3): 179-186. https://doi.org/10.1016/j.eimc.2017.11.013.
- WHO: Global Tuberculosis Report, 2016. Russian. http://www.who.int/tb/publications/global_report/ru.
- Drobot NN, Shevchenko NP, Molchanova NV. Features of the tuberculosis epidemiology – a socially significant disease in children and adolescents under modern conditions. Vyatskiy Meditsinskiy Vestnik 2015; (2): 42-44. Russian. https://elibrary.ru/item.asp?id=23823983.
- Bray F, Znaor A, Cueva P, Korir A, Swaminathan R, Ullrich A, Wang SA, Parkin DM. Planning and developing population-based Cancer registration in low- and middle-income settings. IARC Technical publication No. 43. http://www.iarc.fr/en/publications/pdfs-online/treport-pub/treport-pub43/index.php.
- Toms C, Stapledon R, Coulter C, Douglas P. Tuberculosis notifications in Australia, 2014. Commun Dis Intell Q Rep 2017; 41(3): E247-E263. https://www.ncbi.nlm.nih.gov/pubmed/29720074.
- Korzeniewska-Koseła M. Tuberculosis in Poland in 2015. Przegl Epidemiol 2017; 71(3): 391-403. https://www.ncbi.nlm.nih.gov/pubmed/29182223.
- Stewart RJ, Tsang CA, Pratt RH, Price SF, Langer AJ. Tuberculosis — United States, 2017. MMWR Morb Mortal Wkly Rep 2018; 67(11): 317-323. http://dx.doi.org/10.15585/mmwr.mm6711a2.
- Mason PH, Oni T, MJW van Herpen, Coussens AK. Tuberculosis prevention must integrate technological and basic care innovation. Eur Respir J 2016; 48(5): 1529-1531. https://doi.org/10.1183/13993003.01449-2016.
- Beavers SF, Pascopella L, Davidow AL, Mangan JM, Hirsch-Moverman YR, Golub JE, et al. Tuberculosis epidemiologic studies consortium. tuberculosis mortality in the United States: epidemiology and prevention opportunities. Ann Am Thorac Soc 2018; 15(6): 683–692. https://doi.org/10.1513/AnnalsATS.201705-405OC.
- Jones B, Johnston V, Appuhamy R, Kaczmarek M, Hurwitz M. The epidemiology of tuberculosis in the Australia Capital Territory, 2006-2015. Commun Dis Intell Q Rep 2017; 41(3): E231-E240. https://www.ncbi.nlm.nih.gov/pubmed/29720072.
- Pescarini JM, Simonsen V, Ferrazoli L, Rodrigues LC, Oliveira RC, Waldman EA, Houben R. Migration and tuberculosis transmission in a middle-income country: a cross-sectional study in a central area of São Paulo, Brazil. BMC Med 2018; 16: 62. https://doi.org/10.1186/s12916-018-1055-1.
- Sotgiu G, Beer N, Aliberti S, Migliori GB, van der Werf MJ. Fighting tuberculosis in the U/EEA: towards the new European Union standards on tuberculosis care. Eur Respir J 2016; 48(5): 1278-1281. https://dx.doi.org/10.1183/13993003.01459-2016.
Received 25 June 2018, Revised 17 October 2018, Accepted 21 January 2019
© 2018, Urazayeva S.T., Turegaliyeva Zh.T., Tussupkalieva K.Sh., Begalin T.B., Murzagaliyeva A.Zh., Nurmaganbetova G.Zh., Tashimova Zh.K., Amanshiyeva A.A.
© 2018, Russian Open Medical Journal
Correspondence to Saltanat Urazayeva. Address: Epidemiology Department, West Kazakhstan Marat Ospanov State Medical University, 68, Maresyev str., 030019, Aktobe, Kazakhstan. E-mail: s.urazaeva@mail.ru. Phone: +7(7132)563425. Mob.: +77014651464.

