Introduction
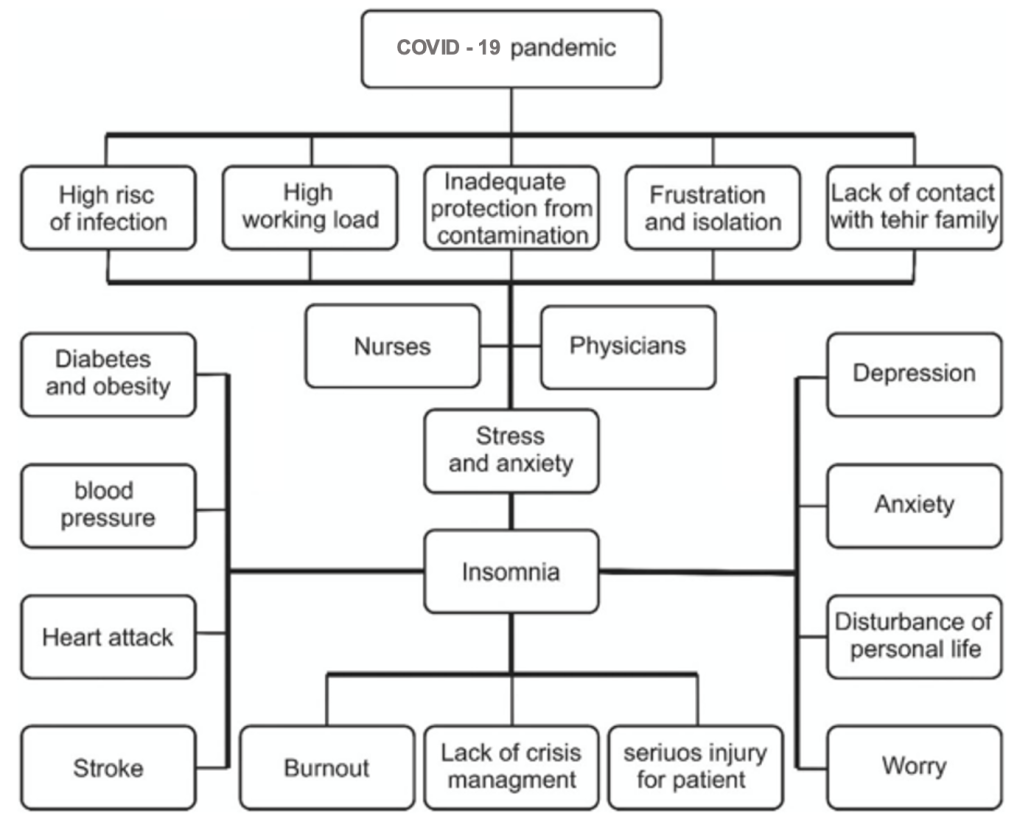
Currently, the impact of the COVID-19 pandemic on the physical and mental health of medical personnel, working in COVID-hospitals, is being widely discussed [1]. The COVID-19 pandemic is a relatively new type of stress factor or trauma from a psychopathological point of view [2]. Despite the existing clinical guidelines for medical workers, who are under increased emotional stress during the COVID-19 pandemic, the problem of sleep disorders associated with the intensive and shift work of medical personnel and chronic distress is actively studied and is not solved to date [3, 4]. Thus, COVID-19 had become not only a serious infectious attack [5, 6], but also led to an increase in neurological disorders both among the general population [7, 8], and healthcare workers during the COVID-19 pandemic (Figure 1).
Figure 1. The impact of the COVID-19 pandemic on sleep disorders among medical personnel [9].
The mental health of medical staff is necessary for the fight against COVID-19, but sometimes it is difficult to be achieved [10-16]. Researchers have proved that risk factors such as marital status, gender, age, social support play crucial role in the mental health of healthcare workers [17-19]. Also, there are other factors that are important for the development of sleep disorders among healthcare workers, such as psychosocial risks associated with health problems [20], work accidents [21, 22], low job satisfaction, low work engagement [23], burnout syndrome [24, 25] and stress related to intensive work during the COVID-19 pandemic [26]. Based on these studies, coping strategies were suggested. For instance, social support can improve the mental health of medical staff, who treat patients with COVID-19, and reduce the risk of sleep disorders, associated economic losses, unintentional medical errors and reduced working efficiency [27-29].
To analyze studies on the prevalence and nature of sleep disorders among healthcare workers during the COVID-19 pandemic.
Material and Methods
This review includes available full-text publications obtained as a result of a literary search in domestic (E-Library) and foreign databases (PubMed, Scopus, Oxford University Press, Springer, Web of Science Core Collection). The search was limited to studies published in 2019-2021.
We used the following keywords to select the publications: pandemic, coronavirus, COVID-19, circadian rhythm sleep disorders, insomnia, medical personnel, doctors, nurses.
In general, we studied domestic and foreign databases and identified 94 publications about the development of sleep disorders among healthcare workers during COVID-19 pandemic in 2000-2021. However, only 88 of these publications reflected the aim of the review. We included 75 full-text publications in this review.
Results
Medical personnel, including doctors, and nurses [30], as well as medical students and caregivers of COVID-19 patients [31], are potentially at risk of developing sleep disorders that can negatively affect their daily life and efficiency, including an increased risk of unintentional medical errors [32, 33]. This is primarily due to the fact that medical personnel, working in COVID-hospitals, experience psychological conflicts, being torn between the responsibilities of caring and treating infected patients and ensuring their own safety. As a result of the growing number of COVID-19 infection cases among their colleagues, the development and impact of psychological distress on these people has become significant [34-37].
Sleep disorders due to psychological distress, disorders of the circadian rhythm due to the shift and stressful work, as well as the development of anxiety and depressive disorders, are the most common neurological symptoms for healthcare workers, who are in direct contact with COVID patients (Table 1) [38, 39], and territorial hospitals [40-44].
Table 1. Prevalence of sleep disorders in medical personnel during the COVID-19 pandemic
|
Nation |
Number of participants |
Study description |
The incidence of sleep disorders (%) |
References |
|
China
|
5,461 medical workers; 1,505 (29.9%) men and 3,956 (70.1%) women. |
Insomnia Severity Index |
20.05% |
[46] |
|
1,257 medical workers, 493 (39.2%) physicians; 764 (60.8%) nurses. |
Insomnia Severity Index |
34.0% |
[13] |
|
|
1,563 medical workers |
Insomnia Severity Index |
36.1% |
[45] |
|
|
100 nurses |
Pittsburgh Sleep Quality Index |
60% |
[55] |
|
|
1,931 nurses |
Pittsburgh Sleep Quality Index |
18.4% |
[56] |
|
|
274 doctors |
The Pittsburgh Sleep Quality Index |
38% |
[50] |
|
|
2,001 medical workers |
Pittsburgh Sleep Quality Index |
61.6% |
[47] |
|
|
33,062 medical workers |
Athens Insomnia Scale Insomnia Severity Index Pittsburgh Sleep Quality Index |
38.8% |
[92] |
|
|
India |
100 doctors |
Experimental scale |
30% |
[51] |
|
Iraq |
268 doctors |
Athens Insomnia Scale |
68.3% |
[52] |
|
Meta analysis (China, Iraq) |
5,868 medical workers, of which: 2,123 doctors; 3,745 nurses |
Athens Insomnia Scale Insomnia Severity Index Pittsburgh Sleep Quality Index |
41.6% |
[9] |
|
Russian |
812 medical workers |
Subjective assessment of sleep quality |
37.4 % |
[48] |
|
500 medical workers |
Subjective assessment of sleep quality |
18.1% |
[49] |
|
|
Oman |
1,139 doctors |
Insomnia Severity Index |
18.5% |
[13] |
|
Turkey |
939 medical workers |
Insomnia Severity Index |
50.4% |
[93] |
|
Bangladesh |
370 doctors |
Sleep Condition Indicator |
18.6% |
[54] |
|
Spain |
100 medical workers |
Epworth Sleepiness Scale Pittsburgh Sleep Quality Index Insomnia Severity Index |
47.65 % |
[94] |
|
Bahrain |
257 medical workers |
Pittsburgh Sleep Quality Index |
75.2% |
[44] |
Sleep disorders among medical workers during the COVID-19 pandemic
According to the Southern Medical University (Guangzhou, China) [45], the prevalence of insomnia among medical personnel during COVID-19 pandemic was 36.1%.
In another Chinese study, conducted by Lin L. Y., Wang J. et. al. [46], using an online questionnaire with the Insomnia Severity Index, a sample of 5,461 medical workers from February 5, 2020 to February 23, 2020 revealed that the prevalence of clinical insomnia during the COVID-19 outbreak was 20.05% (1,131 people).
In a study by Wang W., Song W. et.al [47], the authors analyzed 2,737 questionnaires of healthcare workers from March 4 to March 9, 2020. The Pittsburgh Sleep Quality Index was used as a questionnaire for the sleep study. It was found that during the analyzed period, 61.6% of respondents had sleep disorders. Medical staff, working in COVID-hospitals, were more prone to serious sleep disorders compared to those, who did not work in COVID conditions.
Jahrami H., BaHammam A.S. et.al. [44], analyzed the questionnaires of 280 healthcare workers from several institutions, belonging to the Ministry of Health of Bahrain. They used an online questionnaire based on the Pittsburgh Sleep Quality Index. 75.2% of respondents had sleep disorders.
A cross-sectional study was conducted with the participation of 812 medical workers from 77 regions of Russia, including doctors and nurses, working during the COVID-19 pandemic [48]. In addition to assessing anxiety and depression, this study evaluated the quality of respondents' sleep on a subjective scale from 0 to 10 (where 0 is a severe sleep disorder, 10 is the quality of sleep is not disturbed). The results of the survey showed that 37.4% of medical workers (305 people) had a sleep disorder (maximum severity: up to 5 points).
The Union for the Protection of Mental Health and the Scientific and Educational Center for Modern Medical Technologies conducted comprehensive domestic survey on the psychological state of healthcare workers during the COVID-19 pandemic [49]. More than 500 people participated in this survey. The participants were doctors, nurses, university staff, junior medical staff from 66 regions of Russia. According to the subjective assessment of sleep quality, 18.1% rated sleep quality disorders from 0 to 3 points, while only 3.7% of the surveyed medical workers experienced a severe sleep disorder.
Sleep disorders among doctors during the COVID-19 pandemic
In a study, conducted in Hubei Province (China) from February 26 to March 3, 2020, among doctors (a total of 274 people) working during the COVID-19 pandemic [50], data from a survey, using the Pittsburgh Sleep Quality Index, were presented. The questionnaire contained 19 questions for subjective self-assessment of sleep quality. Sleep disorders were detected in 38% of participants, who scored more than 5 points on the Pittsburgh Sleep Quality Scale.
The Indian study, conducted among practicing orthopedic surgeons (100 people) [51], using an experimental sleep quality scale (from 0 to 10 points, where 10 is the best result), a decrease in sleep quality was detected in 30% of cases.
Iraqi researchers [52] tested patients according to the Athens Insomnia Scale. The scale was a psychometric sleep self-assessment tool, based on the criteria established by the International Classification of Diseases (ICD-10). The scale contained 8 points for assessing falling asleep, night and early morning awakening, sleep time, sleep quality. A total of 268 doctors participated in the study, including surgeons, general practitioners, and internists. Sleep disorders were detected in 68.3% of doctors participating in this study during the COVID-19 outbreak.
In Oman, a study was conducted on the sleep quality in 1,139 doctors working during the COVID-19 from April 8 to April 17, 2020 [53]. They conducted the study using an online questionnaire of the Insomnia Severity Index. A total of 1,167 questionnaires of respondents were received, 28 of which were not completed. Thus, only 1,139 questionnaires were used for further analysis. As a result, it was revealed that 18.5% of doctors during the COVID-19 pandemic noted a violation of the sleep quality.
Another study was conducted in Bangladesh: 370 subjects (doctors working during the COVID-19 pandemic) [54], answered to an online questionnaire of a two-position version of the sleep status indicator, and sleep disorders were detected in 18.6% of respondents.
Sleep disorders among nurses during the COVID-19 pandemic
In order to analyze the sleep quality in nurses working during the COVID-19 pandemic, a study was conducted in Wuhan (China) [55] using the Pittsburgh Sleep Quality Index. In general, among the 100 participants, 60% (60 nurses), according to the questionnaire, had low sleep quality.
Another study conducted in Liaoning Province (China) from February 21 to 23, 2020 [56], using the Pittsburgh Sleep Quality Index, showed that among 1,931 nurses, 18.4% suffered from sleep disorders.
Sleep disorders among medical students in during the COVID-19 pandemic
We analyzed a study conducted among medical students of the King Saud University's College of Medicine, Riyadh, Saudi Arabia during the COVID-19 epidemic [57]. The total number of participants was 453 people from the 3rd to the 5th year of training. The study used the Insomnia Severity Index Scale. According to the results, 162 (34.9%) participants had symptoms of insomnia.
In another study conducted in Umm Al-Qura (Saudi Arabia) during the COVID-19 epidemic [58], among 438 medical students in the 2-6 year of study, 73.7% of respondents had sleep disorders.
In three similar studies conducted in China among medical students during the COVID-19 pandemic [59-62] symptoms of sleep disorders were found in 13.5-44.13%, according to various authors.
A study was conducted among medical students from the 1st to 4th year of study in Kathmandu (Nepal) from January 13, 2021 to February 15, 2021 [63]. The researchers used the Pittsburgh Sleep Quality Index in the Google form. Google forms were sent out by email to 190 respondents, but only 168 respondents returned the completed forms. The survey revealed that 30.36% (n=51) of respondents had low sleep quality.
In studies conducted in Indonesia and Morocco [64, 65] among medical students during COVID-19, sleep disorders were detected in 44.6% and 62.6% of cases, respectively.
According to the studies of medical students conducted in the Russian Federation [66-67] using various sleep quality questionnaires, sleep disorders were detected in 35%, 26.4% and 43.4% according to various authors.
Discussion
We analyzed 18 studies, including foreign and Russian publications (Table 1). The frequency of sleep disorders among healthcare workers during the COVID-19 varied from 20.05% [46] to 75.2% [44]. The mean frequency of occurrence was 44.28±15.45 %.
Of the 18 articles we analyzed, 5 studies were about sleep disorders among doctors (Table 1). The frequency of occurrence of sleep disorders varied from 18.5% to 68.3%. The mean frequency of occurrence was 35.57±16.96%.
Of the 18 articles we analyzed, 2 were devoted to the study of sleep disorders among nurses (Table 1). The frequency of occurrence of sleep disorders varied from 18.4% to 41.6%. The mean frequency of occurrence was 38.65±17.23%.
We have found and analyzed 12 studies, including foreign and Russian publications (Table 2). The frequency of occurrence of sleep disorders among students working in COVID-19 varied from 13.5% to 73.7% [61]. The mean frequency of occurrence was 39.48±15.4%.
Table 2. Prevalence of sleep disorders among students during the COVID-19 pandemic
|
Nation |
Number of participants |
Study description |
The incidence of sleep disorders |
References |
|
Saudi Arabia |
453 |
Insomnia Severity Index |
34.9% |
[57] |
|
438 |
Sleep-50 |
73.7% |
[58] |
|
|
China |
1,026 |
Modified Chinese version of Pittsburgh Sleep Quality Index Scale |
33.2% |
[59] |
|
606 |
Insomnia Severity Index |
32.0% |
[60] |
|
|
3,092 |
Self-Rating Scale of Sleep |
13.5% |
[61] |
|
|
29,663 |
Insomnia Severity Index |
44.13% |
[62] |
|
|
Nepal |
168 |
Pittsburgh Sleep Quality Index Scale |
30.36% |
[63] |
|
Indonesia |
101 |
Insomnia Severity Index |
44.6% |
[64] |
|
Morocco |
549 |
Insomnia Severity Index |
62.6% |
[65] |
|
Russian |
110 |
Psycho-COVID‑19 Questionnaire of psychoemotional state and sleep disorders |
26.4% |
[66] |
|
159 |
Insomnia Severity Index |
43.4% |
[67] |
Sleep disorders during the COVID-19 pandemic are closely associated with high levels of related anxiety, alcohol or drug use and suicidal thoughts [68]. Sleep disorders can also cause adverse consequences for the mental, social and cognitive functioning of healthcare workers, which leads to a deterioration in the overall life quality and a decrease in working efficiency [69, 70].
A study, conducted by Huang Y.E. and Zhao N. [41], reported an increase in the prevalence of sleep disorders among healthcare workers during the COVID-19, which was significantly higher than the prevalence of sleep disorders among other groups of people.
It is known that sleep disorders are one of the crucial problems in the field of public health. This disorder negatively affects the life quality of millions of people around the world [71, 72]. Lack of sleep has a significant negative impact on personal life and leads to a decrease in physical activity [73, 74]. Sleep disorders are associated with various physical complications, including an increased risk of obesity, diabetes, high blood pressure, increased heart rate, heart attack and stroke [75]. On the other hand, high-quality sleep can quickly improve the body functioning, relieve fatigue associated with work, maintain energy levels and mental health [76, 77]. Due to the nature of the working conditions of nurses and doctors during COVID-19 (consecutive work shifts), sleep disorders are highly common among medical personnel and cause a number of psychological disorders in the daily activities of these groups of people [78, 79].
The decrease in workforce productivity among healthcare workers associated with insomnia often has serious irreversible consequences. For instance, due to fatigue, errors that lead to the death of the patient may occur [80, 81]. Moreover, sleep disorders increase the symptoms of burnout, which greatly affects the efficiency of medical workers in critical situations [16].
Compared to previous epidemics, the COVID-19 pandemic may be more complex due to some of its features. These are high contagiousness, rather low level of knowledge about the course of infection and its long-term consequences, as well as the lack of established methods of effective treatment or vaccination [82-84]. In addition, for most hospitals around the world, this is an unprecedented scenario, which is accompanied by great problems in relation to various aspects of healthcare-hygiene concepts, measures and equipment necessary for protection, and the expansion of intensive care units, etc [85, 86]. In addition to short-term psychological stress, it has been shown that factors such as quarantine, work in high-risk wards and contact with infected patients are associated with long-term post-traumatic symptoms during the COVID-19 pandemic [87]. Recent studies report that health workers, fearing being infected, felt stigmatized [88] and had sleep disorders [13, 89-94].
Medical personnel during the COVID-19 pandemic do not have the opportunity to take therapy aimed at combating the symptoms of sleep disorders, due to the need to maintain sufficient attention and the risk of developing excessive drowsiness while on duty in a COVID hospital. The latter can have a negative impact on their professional activities. Hence, this problem certainly requires professional psychotherapeutic correction. Unfortunately, not all medical institutions have such specialists.
Conclusion
Based on the literature review, we discovered out that healthcare professionals had a high risk of developing sleep disorders. These included disorders of their circadian rhythm, a decrease in the quality and duration of night sleep, daytime hypersomnia caused by shift. An additional factor affecting the frequency and severity of sleep disorders in healthcare workers (physicians and nurses) was chronic stress, the importance of which has increased during the COVID-19 pandemic. Currently, the above problem has not been completely solved and requires further research and the development of new programs to help medical personnel.
Conflict of interest
None declared.
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 2020; 395(10227): 912-920. https://doi.org/10.1016/s0140-6736(20)30460-8.
- Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry 2020; 7(3): e14. https://doi.org/10.1016/s2215-0366(20)30047-x.
- Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin Neurosci 2020; 74(4): 281-282. https://doi.org/10.1111/pcn.12988.
- Serrano-Ripoll MJ, Meneses-Echavez JF, Ricci-Cabello I, Fraile-Navarro D, Fiol-deRoque MA, Pastor-Moreno G, et al. Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review and meta-analysis. J Affect Disord 2020; 277: 347-357. https://doi.org/10.1016/j.jad.2020.08.034.
- Jin YH, Huang Q, Wang YY, Zeng XT, Luo LS, Pan ZY, et al. Perceived infection transmission routes, infection control practices, psychosocial changes, and management of COVID-19 infected healthcare workers in a tertiary acute care hospital in Wuhan: a cross-sectional survey. Mil Med Res 2020; 7(1): 24. https://doi.org/10.1186/s40779-020-00254-8.
- Luo LS, Jin YH, Cai L, Pan ZY, Zeng XT, Wang XH. COVID-19: Presumed Infection Routes and Psychological Impact on Staff in Administrative and Logistics Departments in a Designated Hospital in Wuhan, China. Front Psychol 2020; 11: 1501. https://doi.org/10.3389/fpsyg.2020.01501.
- Du J, Mayer G, Hummel S, Oetjen N, Gronewold N, Zafar A, et al. Mental Health Burden in Different Professions During the Final Stage of the COVID-19 Lockdown in China: Cross-sectional Survey Study. J Med Internet Res 2020; 22(12): e24240. https://doi.org/10.2196/24240.
- Fardin MA. COVID-19 and Anxiety: A Review of Psychological Impacts of Infectious Disease Outbreaks. Arch Clin Infect Dis 2020. 15(COVID-19): e102779; http://doi.org/10.5812/archcid.102779.
- Salari N, Khazaie H, Hosseinian-Far A, Ghasemi H, Mohammadi M, Shohaimi S, et al. The prevalence of sleep disturbances among physicians and nurses facing the COVID-19 patients: a systematic review and meta-analysis. Global Health 2020; 16(1): 92. https://doi.org/10.1186/s12992-020-00620-0.
- Kang L, Ma S, Chen M, Yang J, Wang Y, Li R, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav Immun 2020; 87: 11-17. https://doi.org/10.1016/j.bbi.2020.03.028,
- Juan Y, Yuanyuan C, Qiuxiang Y, Cong L, Xiaofeng L, Yundong Z, et al. Psychological distress surveillance and related impact analysis of hospital staff during the COVID-19 epidemic in Chongqing, China. Compr Psychiatry 2020; 103: 152198. https://doi.org/10.1016/j.comppsych.2020.152198.
- Moreno C, Wykes T, Galderisi S, Nordentoft M, Crossley N, Jones N, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry 2020; 7(9): 813-824. https://doi.org/10.1016/s2215-0366(20)30307-2.
- Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open 2020; 3(3): e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976.
- Cai H, Tu B, Ma J, Chen L, Fu L, Jiang Y, et al. Psychological Impact and Coping Strategies of Frontline Medical Staff in Hunan Between January and March 2020 During the Outbreak of Coronavirus Disease 2019 (COVID-19) in Hubei, China. Med Sci Monit 2020; 26: e924171. https://doi.org/10.12659/msm.924171.
- Liang Y, Chen M, Zheng X, Liu J. Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J Psychosom Res 2020; 133: 110102. https://doi.org/10.1016/j.jpsychores.2020.110102.
- Xiao H, Zhang Y, Kong D, Li S, Yang N. The Effects of Social Support on Sleep Quality of Medical Staff Treating Patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit 2020; 26: e923549. https://doi.org/10.12659/msm.923549.
- Chen SH, Liu JE, Bai XY, Yue P, Luo SX. Providing targeted psychological support to frontline nurses involved in the management of COVID-19: An action research. J Nurs Manag 2021; 29(5): 1169-1179. https://doi.org/10.1111/jonm.13255.
- European Agency for Safety and Health at Work, Nielsen K, Jorgensen MB, Milczarek M, Munar L. Healthy workers, thriving companies. A practical guide to well-being at work: tackling psychosocial risks and musculoskeletal disorders in small businesses. Luxembourg: Publications Office 2019; 102 p. https://doi.org/10.2802/237140.
- Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One 2020; 15(4): e0231924. https://doi.org/10.1371/journal.pone.0231924.
- Bergh LIV, Leka S, Zwetsloot GIJM. Tailoring Psychosocial Risk Assessment in the Oil and Gas Industry by Exploring Specific and Common Psychosocial Risks. Saf Health Work 2018; 9(1): 63-70. https://doi.org/10.1016/j.shaw.2017.05.001.
- Fornell B, Correa M, López Del Amo MP, Martín JJ. Influence of changes in the Spanish labor market during the economic crisis (2007-2011) on perceived health. Qual Life Res 2018; 27(8): 2095-2105. https://doi.org/10.1007/s11136-018-1824-5.
- Wu X, Li J, Liu G, Liu Y, Cao J, Jia Z. The effects of emotional labor and competency on job satisfaction in nurses of China: A nationwide cross-sectional survey. Int J Nurs Sci 2018; 5(4): 383-389. https://doi.org/10.1016/j.ijnss.2018.08.001.
- Watanabe M, Yamauchi K. Subtypes of overtime work and nurses' fatigue, mental status, and work engagement: A latent class analysis of Japanese hospital nurses. J Adv Nurs 2019; 75(10): 2122-2132. https://doi.org/10.1111/jan.13991.
- Elshaer NS, Moustafa MS, Aiad MW, Ramadan MI. Job stress and burnout syndrome among critical care healthcare workers. Alex J Med 2018; 54: 273-277. https://doi.org/10.1111/jan.13991.
- Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol 2001; 52: 397-422. https://doi.org/10.1146/annurev.psych.52.1.397.
- Junne F, Michaelis M, Rothermund E, Stuber F, Gündel H, Zipfel S, et al. The role of work-related factors in the development of psychological distress and associated mental disorders: Differential views of human resource managers, occupational physicians, primary care physicians and psychotherapists in Germany. Int J Environ Res Public Health 2018; 15(3): 559. https://doi.org/10.3390/ijerph15030559.
- Pedro IC, Rocha SM, Nascimento LC. Social support and social network in family nursing: reviewing concepts. Rev Lat Am Enfermagem 2008; 16(2): 324-327. https://doi.org/10.1590/s0104-11692008000200024.
- Samushiya MA, Ragimova AA, Amosova NA, Smolentseva IG, Oinotkinova OSh, Bonkalo TI, et al. Problems of psycho-emotional well-being of medical personnel working in the context of the COVID-19 pandemic. Annals of the Russian academy of medical sciences 2020; 75(5S): 426-433. Russian. https://doi.org/10.15690/vramn1426.
- Korabelnikova EA, Vorobieva OV, Makarov SA, Danilov AB. Sleep disorders in doctors in the context of the COVID-19 pandemic. Medical Alphabet 2021; (3): 48-56. Russian. https://doi.org/10.33667/2078-5631-2021-3-48-56.
- Paiva CE, Martins BP, Paiva BSR. Doctor, are you healthy? A cross-sectional investigation of oncologist burnout, depression, and anxiety and an investigation of their associated factors. BMC Cancer 2020; 18(1): 1044. https://doi.org/10.1186/s12885-018-4964-7.
- Zerbini G, Ebigbo A, Reicherts P, Kunz M, Messman H. Psychosocial burden of healthcare professionals in times of COVID-19 – a survey conducted at the University Hospital Augsburg. Ger Med Sci 2020; 18: Doc05. https://doi.org/10.3205/000281.
- Kang L, Ma S, Chen M, Yang J, Wang Y, Li R, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav Immun 2020; 87: 11-17. https://doi.org/10.1016/j.bbi.2020.03.028.
- Hummel S, Oetjen N, Du J, Posenato E, Resende de Almeida RM, Losada R, et al. Mental Health Among Medical Professionals During the COVID-19 Pandemic in Eight European Countries: Cross-sectional Survey Study. J Med Internet Res 2021; 23(1): e24983. https://doi.org/10.2196/24983.
- Fu XW, Wu LN, Shan L. Review of possible psychological impacts of COVID-19 on frontline medical staff and reduction strategies. World J Clin Cases 2020; 8(15): 3188-3196. https://doi.org/10.12998/wjcc.v8.i15.3188.
- Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr 2020; 33(2): e100213. https://doi.org/10.1136/gpsych-2020-100213.
- Yifan T, Ying L, Chunhong G, Jing S, Rong W, Zhenyu L, et al. Symptom Cluster of ICU Nurses Treating COVID-19 Pneumonia Patients in Wuhan, China. J Pain Symptom Manage 2020; 60(1): e48-e53. https://doi.org/10.1016/j.jpainsymman.2020.03.039.
- Blake H, Bermingham F, Johnson G, Tabner A. Mitigating the Psychological Impact of COVID-19 on Healthcare Workers: A Digital Learning Package. Int J Environ Res Public Health 2020; 17(9): 2997. https://doi.org/10.3390/ijerph17092997.
- Yaribeygi H, Panahi Y, Sahraei H, Johnston TP, Sahebkar A. The impact of stress on body function: A review. EXCLI J 2017; 16: 1057-1072. https://doi.org/10.17179/excli2017-480.
- Song X, Fu W, Liu X, Luo Z, Wang R, Zhou N, et al. Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China. Brain Behav Immun. 2020; 88: 60-65. https://doi.org/10.1016/j.bbi.2020.06.002.
- Hu Z, Wang H, Xie J, Zhang J, Li H, Liu S. Burnout in ICU doctors and nurses in mainland China-A national cross-sectional study. J Crit Care 2021; 62, 265-270. https://doi.org/10.1016/j.jcrc.2020.12.029.
- Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res 2020; 288: 112954. https://doi.org/10.1016/j.psychres.2020.112954.
- Choi EPH, Hui BPH, Wan EYF. Depression and Anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health 2020; 17(10): 3740. https://doi.org/10.3390/ijerph17103740.
- Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The Fear of COVID-19 Scale: Development and Initial Validation. Int J Ment Health Addict 2022; 20(3): 1537-1545. https://doi.org/10.1007/s11469-020-00270-8.
- Jahrami H, BaHammam AS, AlGahtani H, Ebrahim A, Faris M, AlEid K, et al. The examination of sleep quality for frontline healthcare workers during the outbreak of COVID-19. Sleep Breath 2021; 25(1): 503-511. https://doi.org/10.1007/s11325-020-02135-9.
- Liu S, Yang L, Zhang C, Xiang YT, Liu Z, Hu S, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry 2020; 7(4): e17-e18. https://doi.org/10.1016/s2215-0366(20)30077-8.
- Lin LY, Wang J, Ou-Yang XY, Miao Q, Chen R, Liang FX, et al. The immediate impact of the 2019 novel coronavirus (COVID-19) outbreak on subjective sleep status. Sleep Med 2021; 77: 348-354. https://doi.org/10.1016/j.sleep.2020.05.018.
- Wang W, Song W, Xia Z, He Y, Tang L, Hou J, et al. Sleep Disturbance and Psychological Profiles of Medical Staff and Non-Medical Staff During the Early Outbreak of COVID-19 in Hubei Province, China. Front Psychiatry 2020; 11: 733. https://doi.org/10.3389/fpsyt.2020.00733.
- Bachilo EV, Novikov DE, Efremov AA. Mental health assessment of medical workers during the COVID-19 pandemic in Russia: results of an online survey. Zh Nevrol Psikhiatr Im S S Korsakova 2021; 121(3): 104-109. Russian. https://doi.org/10.17116/jnevro2021121031104.
- Treushnikova NV, Bachilo EV, Borodin VI, Antonova AA. Recommendations for medical workers in conditions of increased psycho-emotional stress during the COVID-19 pandemic. Moscow, Russia: Scientific and Educational Center for Modern Medical Technologies. 2020; 45 p. Russian. https://edu.rosminzdrav.ru/fileadmin/user_upload/specialists/COVID-19/dop-materials/13-5-20/Rekomendacii_dlja_medrabotnikov.pdf.
- Wang LQ, Zhang M, Liu GM, Nan SY, Li T, Xu L, et al. Psychological impact of coronavirus disease (COVID-19) epidemic on medical staff in different posts in China: A multicenter study. J Psychiatr Res 2020; 129: 198-205. https://doi.org/10.1016/j.jpsychires.2020.07.008.
- Sharma V, Kumar N, Gupta B, Mahajan A. Impact of COVID-19 pandemic on orthopaedic surgeons in terms of anxiety, sleep outcomes and change in management practices: A cross-sectional study from India. J Orthop Surg (Hong Kong) 2021; 29(1): 23094990211001621. https://doi.org/10.1177/23094990211001621.
- Abdulah DM, Musa DH. Insomnia and stress of physicians during COVID-19 outbreak. Sleep Med X 2020; 2: 100017. https://doi.org/10.1016/j.sleepx.2020.100017.
- Alshekaili M, Hassan W, Al Said N, Al Sulaimani F, Jayapal SK, Al-Mawali A, et al. Factors associated with mental health outcomes across healthcare settings in Oman during COVID-19: frontline versus non-frontline healthcare workers. BMJ Open 2020; 10(10): e042030. https://doi.org/10.1136/bmjopen-2020-042030.
- Barua L, Zaman MS, Omi FR, Faruque M. Psychological burden of the COVID-19 pandemic and its associated factors among frontline doctors of Bangladesh: a cross-sectional study. F1000Res 2020; 9: 1304. https://doi.org/10.12688/f1000research.27189.3.
- Tu ZH, He JW, Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak. Medicine (Baltimore) 2020; 99(26): e20769. https://doi.org/10.1097/md.0000000000020769.
- Zhou Y, Yang Y, Shi T, Song Y, Zhou Y, Zhang Z, et al. Prevalence and Demographic Correlates of Poor Sleep Quality Among Frontline Health Professionals in Liaoning Province, China During the COVID-19 Outbreak. Front Psychiatry 2020; 11: 520 https://doi.org/10.3389/fpsyt.2020.00520.
- Alrashed FA, Sattar K, Ahmad T, Akram A, Karim SI, Alsubiheen AM. Prevalence of insomnia and related psychological factors with coping strategies among medical students in clinical years during the COVID-19 pandemic. Saudi J Biol Sci 2021; 28(11): 6508-6514. https://doi.org/10.1016/j.sjbs.2021.07.022.
- Abdelmoaty Goweda R, Hassan-Hussein A, Ali Alqahtani M, Janaini MM, Alzahrani AH, Sindy BM, et al. Prevalence of sleep disorders among medical students of Umm Al-Qura University, Makkah, Kingdom of Saudi Arabia. J Public Health Res 2021; 9(Suppl 1): 2020. https://doi.org/10.4081/jphr.2020.1921.
- Xie J, Li X, Luo H, He L, Bai Y, Zheng F, et al. Depressive Symptoms, Sleep Quality and Diet During the 2019 Novel Coronavirus Epidemic in China: A Survey of Medical Students. Front Public Health 2021; 8: 588578. https://doi.org/10.3389/fpubh.2020.588578.
- Liu D, Liu S, Zhu L, Li D, Huang D, Deng H, et al. Prevalence and Related Factors of Insomnia Among Chinese Medical Staff in the Middle and Late Stage of COVID-19. Front Psychiatry 2020; 11: 602315. https://doi.org/10.3389/fpsyt.2020.602315.
- Wang X, Chen H, Liu L, Liu Y, Zhang N, Sun Z, et al. Anxiety and Sleep Problems of College Students During the Outbreak of COVID-19. Front Psychiatry 2020; 11: 588693. https://doi.org/10.3389/fpsyt.2020.588693.
- Liu Z, Liu R, Zhang Y, Zhang R, Liang L, Wang Y, et al. Association between perceived stress and depression among medical students during the outbreak of COVID-19: The mediating role of insomnia. J Affect Disord 2021; 292: 89-94. https://doi.org/10.1016/j.jad.2021.05.028.
- Shrestha D, Adhikari SP, Rawal N, Budhathoki P, Pokharel S, Adhikari Y, et al. Sleep quality among undergraduate students of a medical college in Nepal during COVID-19 pandemic: an online survey. F1000Res 2021; 10: 505. https://doi.org/10.12688/f1000research.53904.2.
- Mazza MG, De Lorenzo R, Conte C, Poletti S, Vai B, Bollettini I, et al. COVID-19 BioB Outpatient Clinic Study group, Benedetti F. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav Immun 2020; 89: 594-600. https://doi.org/10.1016/j.bbi.2020.07.037.
- Essangri H, Sabir M, Benkabbou A, Majbar MA, Amrani L, Ghannam A, et al. Predictive Factors for Impaired Mental Health among Medical Students during the Early Stage of the COVID-19 Pandemic in Morocco. Am J Trop Med Hyg 2021; 104(1): 95-102 https://doi.org/10.4269/ajtmh.20-1302.
- Litvinova AA, Kravtsiva AV, Asmolovsky AV, Shamatkova SV. Features of the psychoemotional state of doctors providing medical care in the context of the COVID-19 pandemic. Clinical Medicine (Russian Journal) 2021; 99(2): 103-107. Russian. https://doi.org/10.30629/0023-2149-2021-99-2-103-107.
- Tkachenko NV, Abaeva AB, Chervonny MO, Kivva AA. Determination of mental health indicators of medical students working in the healthcare sector in the context of the Covid-19 pandemic. Student 2021; 4(1): 39. Russian. https://www.elibrary.ru/item.asp?id=44654326.
- Lee SA. Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death Stud 2020; 44(7): 393-401. https://doi.org/10.1080/07481187.2020.1748481.
- Szentkirályi A, Madarász CZ, Novák M. Sleep disorders: impact on daytime functioning and quality of life. Expert Rev Pharmacoecon Outcomes Res 2009; 9(1): 49-64. https://doi.org/10.1586/14737167.9.1.49.
- Zhang C, Yang L, Liu S, Ma S, Wang Y, Cai Z, et al. Survey of Insomnia and Related Social Psychological Factors Among Medical Staff Involved in the 2019 Novel Coronavirus Disease Outbreak. Front Psychiatry 2020; 11: 306. https://doi.org/10.3389/fpsyt.2020.00306.
- Léger D, Bayon V. Societal costs of insomnia. Sleep Med Rev. 2010; 14(6): 379-389. https://doi.org/10.1016/j.smrv.2010.01.003.
- Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry 2020; 63(1): e32. https://doi.org/10.1192/j.eurpsy.2020.35.
- Kousloglou S, Mouzas O, Bonotis K, Roupa Z, Vasilopoulos A, Angelopoulos N. Insomnia and burnout in Greek Nurses. Hippokratia 2014; 18(2): 150-155. https://pubmed.ncbi.nlm.nih.gov/25336879/.
- Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet 2020; 395(10223): 470-473. https://doi.org/10.1016/s0140-6736(20)30185-9.
- Silva-Costa A, Griep RH, Rotenberg L. Associations of a Short Sleep Duration, Insufficient Sleep, and Insomnia with Self-Rated Health among Nurses. PLoS One 2015; 10(5): e0126844. https://doi.org/10.1371/journal.pone.0126844.
- Cao XL, Wang SB, Zhong BL, Zhang L, Ungvari GS, Ng CH, et al. The prevalence of insomnia in the general population in China: A meta-analysis. PLoS One 2017; 12(2): e0170772. https://doi.org/10.1371/journal.pone.0170772.
- Wu K, Wei X. Analysis of Psychological and Sleep Status and Exercise Rehabilitation of Front-Line Clinical Staff in the Fight Against COVID-19 in China. Med Sci Monit Basic Res 2020; 26: e924085. https://doi.org/10.12659/msmbr.924085.
- Yazdi Z, Sadeghniiat-Haghighi K, Javadi AR, Rikhtegar G. Sleep quality and insomnia in nurses with different circadian chronotypes: morningness and eveningness orientation. Work 2014; 47(4): 561-567. https://doi.org/10.3233/wor-131664.
- Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord 2011; 135(1-3): 10-19. https://doi.org/10.1016/j.jad.2011.01.011.
- Lee AM, Wong JG, McAlonan GM, Cheung V, Cheung C, Sham PC, et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry 2007; 52(4): 233-240. https://doi.org/10.1177/070674370705200405.
- Sher L. COVID-19, anxiety, sleep disturbances and suicide. Sleep Med 2020; 70: 124. https://doi.org/10.1016/j.sleep.2020.04.019.
- Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic – A review. Asian J Psychiatr 2020; 51: 102119. https://doi.org/10.1016/j.ajp.2020.102119.
- Dong ZQ, Ma J, Hao YN, Shen XL, Liu F, Gao Y. The social psychological impact of the COVID-19 pandemic on medical staff in China: A cross-sectional study. Eur Psychiatry 2020; 63(1): e65. https://doi.org/10.1192/j.eurpsy.2020.59.
- Geoffroy PA, Le Goanvic V, Sabbagh O, Richoux C, Weinstein A, Dufayet G, et al. Psychological Support System for Hospital Workers During the Covid-19 Outbreak: Rapid Design and Implementation of the Covid-Psy Hotline. Front Psychiatry 2020; 11: 511. https://doi.org/10.3389/fpsyt.2020.00511.
- Short NA, Raines AM, Oglesby ME, Zvolensky MJ, Schmidt NB. Insomnia and emotion dysregulation: independent and interactive associations with posttraumatic stress symptoms among trauma-exposed smokers. J Affect Disord 2014; 165: 159-165. https://doi.org/10.1016/j.jad.2014.04.069.
- Sinha SS. Trauma-induced insomnia: A novel model for trauma and sleep research. Sleep Med Rev 2016; 25: 74-83. https://doi.org/10.1016/j.smrv.2015.01.008.
- Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry 2009; 54(5): 302-311. https://doi.org/10.1177/070674370905400504.
- Bai Y, Lin CC, Lin CY, Chen JY, Chue CM, Chou P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv 2004; 55(9): 1055-1057. https://doi.org/10.1176/appi.ps.55.9.1055.
- Shah K, Chaudhari G, Kamrai D, Lail A, Patel RS. How Essential Is to Focus on Physician's Health and Burnout in Coronavirus (COVID-19) Pandemic? Cureus 2020; 12(4): e7538. https://doi.org/10.7759/cureus.7538.
- Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ 2020; 369: m1642. https://doi.org/10.1136/bmj.m1642.
- Shanafelt T, Ripp J, Trockel M. Understanding and Addressing Sources of Anxiety Among Health Care Professionals During the COVID-19 Pandemic. JAMA 2020; 323(21): 2133-2134. https://doi.org/10.1001/jama.2020.5893.
- Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun 2020; 88: 901-907. https://doi.org/10.1016/j.bbi.2020.05.026.
- Şahin MK, Aker S, Şahin G, Karabekiroğlu A. Prevalence of Depression, Anxiety, Distress and Insomnia and Related Factors in Healthcare Workers During COVID-19 Pandemic in Turkey. J Community Health 2020; 45(6): 1168-1177. https://doi.org/10.1007/s10900-020-00921-w.
- Herrero San Martin A, Parra Serrano J, Diaz Cambriles T, Arias Arias EM, Muñoz Méndez J, Del Yerro Álvarez MJ, et al. Sleep characteristics in health workers exposed to the COVID-19 pandemic. Sleep Med 2020; 75: 388-394. https://doi.org/10.1016/j.sleep.2020.08.013.
Received 28 September 2021, Revised 19 March 2022, Accepted 17 May 2022
© 2021, Russian Open Medical Journal
Correspondence to Vladislav E. Karnaukhov. Address: Partizan Zheleznyak Street 1, Krasnoyarsk, 660022, Russia. Phone: +79835000484. E-mail: karnauhov.vlad@mail.ru.